Throughout 2024-2025, Research Manitoba celebrates our 10th anniversary year. As we mark this achievement, we will be looking back at some of our past funded researchers to highlight their success.
Breathe easy: One Researcher’s Mission to Prevent Lung Disease Before It Starts.
Profile written by: Brian Cole
Diagnosed with asthma at age six, Dr. Christopher Pascoe is now leading groundbreaking research in Manitoba to uncover how early-life exposures shape lifelong lung health.
“I’ve always had to take medication for it, to varying levels,” Pascoe says in reference to the lung condition that afflicts an estimated 4.6 million Canadians. “Sometimes it is well controlled, sometimes it is not,” he says.But it wasn’t until he was a student at the University of British Columbia some 17 years later that he really started to understand just how much damage asthma can do to a person’s lungs.
At the time, Pascoe, who is now an investigator with the Children’s Hospital Research Institute of Manitoba (CHRIM) and an associate professor in the Department of Physiology and Pathophysiology at the University of Manitoba (UM), had just finished his undergraduate degree and was considering various career paths when he stumbled upon a summer job opportunity.
The Centre for Heart Lung Innovation at St. Paul’s Hospital in Vancouver just happened to be looking for students to analyze images of lungs the centre had received over the years. “They had a bio-bank of all the donor lungs they had gotten, and there was an opportunity to go in and look at images of these lungs under a microscope and… measure how thick were the airways, how much muscle was around it.”
The experience changed Pascoe’s life.
From that moment, Pascoe was determined to learn more about asthma, including what could be done to treat or even prevent the condition from developing in the first place.
“I don’t think I ever went into it thinking, ‘Oh yeah, in my lifetime I will cure asthma,” he says. “But it was just a curiosity about what is happening here in my lungs,” he says, gently tapping his chest.
Today, Pascoe’s lab, which includes four student researchers, is focused on better understanding the environmental and genetic risk factors contributing to various lung diseases, including asthma and chronic obstructive pulmonary disease (COPD).
One example of the work undertaken by Pascoe and his team involves a study, launched in 2021 with support from Research Manitoba, into whether exposure to maternal diabetes could lead to asthma or even COPD in later life. As he explains, scientists have known for some time that a child exposed to cigarette smoke early in life will be at higher risk for lung problems if they, too, choose to smoke as an adult. But Pascoe wanted to dig a little deeper by investigating whether other environmental factors could also leave children at higher risk for lung problems when they got older.
Maternal diabetes seemed like a good place to start, in part because previous studies suggested there could be a link between exposure to it and lung problems in later life among mice. “If you looked at mice that were exposed to diabetes, their airways were narrower… so there were signs there that (the exposure) was changing the lungs and making them more susceptible to asthma, but we wanted to investigate that further,” says Pascoe.
At the same time, Pascoe and his team noticed that in addition to potentially becoming susceptible to asthma, the lab mice also appeared to be more vulnerable to COPD. “COPD is an interesting disease because it is classically thought of as a disease of smokers. But not everybody who smokes gets COPD – about 20 per cent of smokers do, and we really don’t know why. But then also, there is an awareness now that people who have never smoked a day in their life will get COPD. And it seems to be related to poor growth of the lungs, poor functioning of the lungs, leading to a loss of lung function later in life”.
“And maybe the thing that makes two people differentially susceptible to cigarette smoke is the thing they are exposed to in early life… something that makes their body less able to handle and detoxify the cigarette smoke… So the thought was that if we took mice that had been exposed to maternal diabetes, then expose them to cigarette smoke as adults, we could then measure how sensitive they are to that – how much inflammation did they get, how much tissue damage did they get?”
As it turned out, the study found that, yes, exposure to maternal diabetes did change the susceptibility of mice to disease, just not in the way that was expected.
“There was a sex difference,” says Pascoe. “In males, it made the smoke more inflammatory, it seemed to cause more tissue damage. In females, it seemed to have the opposite effect where it seemed to completely suppress the inflammatory response of cigarette smoke.”
Pascoe says he isn’t sure whether the surprising results of the study are a good thing or not.
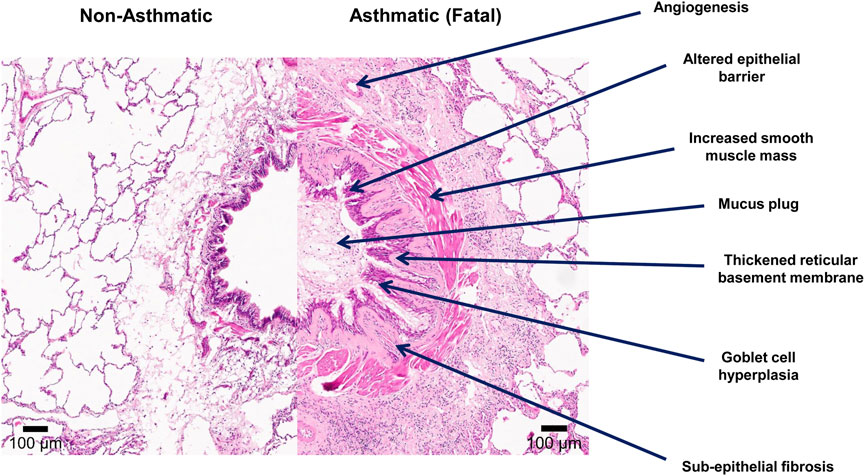
The image above shows a split screen of an asthmatic lung (right) and non-asthmatic lung. The darker colour on the right illustrates the damage done to a lung with asthma.
As he explains, one would assume that if the immune cell that prompts the inflammatory response and subsequent tissue damage could be removed that would be a good thing. “But inflammation in response to cigarette smoke is the body’s natural response. So, maybe it is not good that your body does not go through this process.”
Pascoe’s study builds on existing knowledge in this area.
While previous studies have shown that children exposed to cigarette smoke in utero who go on to smoke as adults are likely to be at higher risk for lung problems, Pascoe’s research shows that other environmental factors, such as maternal diabetes, may also play a role in promoting the development of asthma and COPD. “We’ve seen that maternal diabetes can change the lung in a way that is consistent with asthma. And the interesting thing about lung disease is that if you have severe asthma, you are more likely to get COPD later,” he says.
The results of the study are expected to be published later this year. Meanwhile, Pascoe is using the Research Manitoba funded study to obtain another grant from the Canadian Institute of Health Research (CIHR) to continue with his inquiries in this area.
As he explains, the CIHR grant will allow him to investigate what role airway smooth muscle cells play in the development of lung diseases like asthma and COPD. “It’s a specific cell within the lungs that seems to be a problem in most lung diseases,” he says.
* Determine whether increased levels of cytokines in amniotic fluid can influence changes in lung development and function.
* Explore whether certain microRNAs play a role in the development of asthma.
* Shed light on the role hydroxy eicosatetraenoic acids play in regulating airway smooth muscle physiology.
* Investigate potential links between lung disease and vaping, which has been linked to about 30 teenagers in the United States over the years.
Pascoe is optimistic about the impact his team can have as they continue working towards treating or even preventing lung conditions such as asthma or COPD.
Indeed, some recent clinical trials carried out elsewhere have already shown that high dose vitamin C, which can act as an antioxidant, prevents the development of wheeze (a risk factor for asthma in kids) in mothers who smoke, he says.

Dr. Christopher Pascoe is an assistant professor in the Department of Physiology and Pathophysiology at the University of Manitoba and a principal investigator at the Children’s Hospital Research Institute of Manitoba. He completed his Bachelor of Science in Biology at the University of the Fraser Valley and earned his PhD in Experimental Medicine at the University of British Columbia. In 2017, he was awarded the prestigious Banting Postdoctoral Fellowship. Dr. Pascoe joined the Rady Faculty of Health Sciences as an assistant professor in late 2019.