Written by: Brian Cole

Gloria Vazquez Grande review a patient’s chart in the intensive care unit at Health Sciences Centre.
Treating COVID-19 patients with corticosteroids may reduce mortality by as much as 12 per cent, says a local physician who is supervising several clinical trials on treatments for the disease.
Dr. Ryan Zarychanski, a hematologist, critical care physician and clinician-scientist with the University of Manitoba and CancerCare Manitoba, says studies conducted here and around the world show that corticosteroids are most beneficial for patients with moderate (on oxygen) or severe (requiring a ventilator) disease. However, he also points out the treatment does not appear to help patients with mild symptoms, and may even cause harm in this group of patients.
“Our data from the trials we’ve participated in, combined with the data from six other trials, consistently demonstrate that steroids given to people admitted to hospital, particularly those on oxygen, result in a significant reduction in mortality,” says Zarychanski. As a result, he says, the use of anti-inflammatory steroids is “now the standard of care” for those patients in Manitoba.
The Manitoba corticosteroid clinical trial is one of six studies involving eight therapies that Zarychanski and his team — which includes more than 30 physicians, nurses, research coordinators, investigators, and medical students — have launched this year.

The team’s work has been supported by about $1.4 million in start-up support from the provincial government and Research Manitoba, as well as additional funding from the Manitoba Medical Services Foundation. This initial investment was leveraged by Zarychanski’s team to attract a further $8 million from the Canadian Institutes of Health Research and other national or international funders to lead several trials locally and internationally.
News concerning the benefits of corticosteroids comes amid a recent surge in COVID-19 cases. As of Nov. 3, 246,000 people have been diagnosed with COVID-19 in Canada. About 205,000 people have recovered and 10,328 have died. In Manitoba, 6,377 people have been diagnosed with COVID-19. About 2,797 have recovered from the disease, while 85 have died.
Corticosteroids represent the main treatment that has shown a clear benefit for COVID-19 patients, according to Zarychanski. Patients very early in the course of illness may also receive a small benefit from being treated with an anti-viral called remdesivir, but the clinical relevance of this benefit is still uncertain. Remdesivir is available in Manitoba as part of a World Health Organization international clinical trial.
As it turns out, both corticosteroids and remdesivir were included in the treatment provided recently to United States President Donald Trump, who was diagnosed with COVID-19 earlier this month. Trump also received an experimental cocktail of monoclonal antibodies — a treatment that has not yet been approved for general use. Monoclonal antibodies of the kind that Trump was given may be trialed in Manitoba at some point in the future.
Corticosteroids do not help a patient by attacking COVID-19 infection, per se. Rather, they are used to help better manage the immune system’s efforts to fight infection.
As Zarychanski explains, part of the body’s response to an infection is to mount an inflammatory reaction involving several proteins, one group of which are called cytokines.
“If a person’s inflammatory reaction is too forceful, healthy cells and organs of the infected host can be damaged,” he says. “In essence, the adaptive inflammatory response to an invading pathogen becomes maladaptive and injurious to the patient.” This is known as a “cytokine storm.”
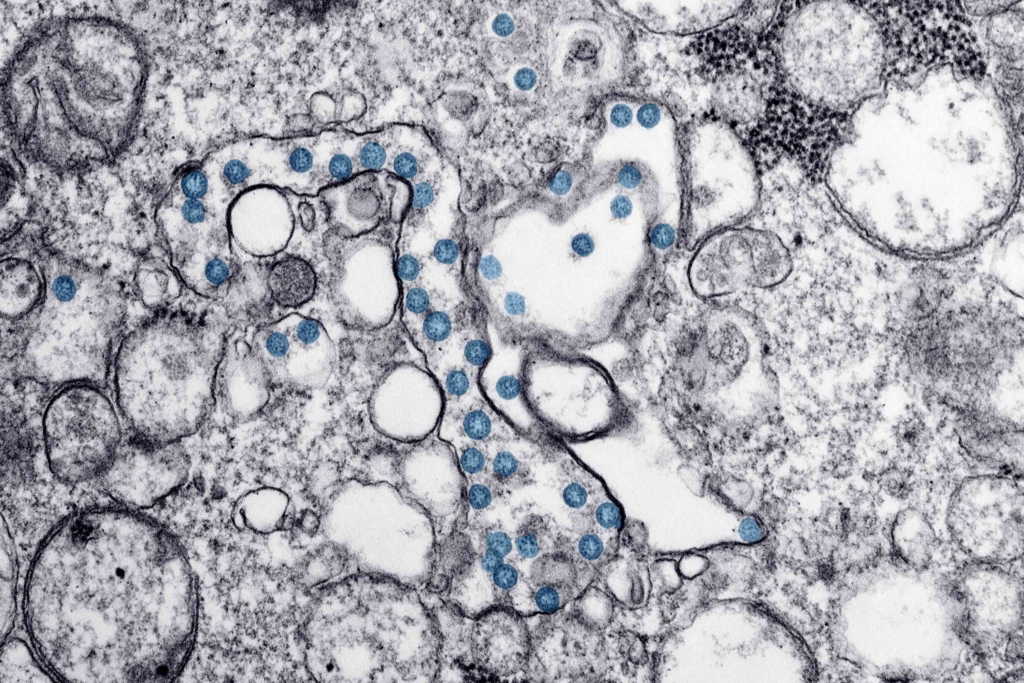
Zarychanski says corticosteroids, of which dexamethasone has been most studied, may act by reducing inflammation associated with the onset of COVID-19 and, in turn, reduce the onset and severity of lung injury or multiple organ failure.
It is important to note, he says, that the steroids in question are anti-inflammatories, not anabolic steroids, which are used to build muscle or dishonestly boost athletic performance.
“There are several different types of steroids,” he says. “The one most studied is called dexamethasone. Other steroids may work just as good, but the majority of the data is with dexamethasone.”
The clinical trial, and the resulting changes in care for COVID-19 patients, shows how clinical research can play in important role in improving treatment for deadly disease in real time.
Indeed, the introduction of new drug therapies may be one reason why mortality rates among critically ill patients with COVID-19 seem to be declining even as cases of COVD-19 surge in most parts of the country, a point confirmed by two recent studies. Zarychanski says factors in the decline include small tweaks in the way care is provided (ventilating some patients on their stomach as opposed to their back to improve oxygenation) and the fact that caseloads seems to be shifting to include more younger Canadians, who are less likely than older patients to die from COVID-19. The latter could also be tempering hospitalization rates because younger patients may be able to recover at home.
In addition to identifying treatments that work, Zarychanski and his team have also shown that some treatments do not appear to be effective in treating COVID-19. These include hydroxychloroquine (used to treat autoimmune conditions such as lupus and rheumatoid arthritis) and Lopinavir/ritonavir (also known as Keletra and used to treat patients with HIV infection), and Interferon beta-1a, an immune modulator that is used to treat patients with multiple sclerosis.
Meanwhile, the team has recently launched a clinical trial using convalescent plasma, which involves collecting plasma from people who have recovered from COVID-19 and giving it to patients who are sick with the disease. This trial is part of a pan-Canadian trial funded by the Canadian Institutes of Health Research. Zarychanski is leading a similar trial of convalescent plasma given to critically ill patients.
Another potentially promising clinical trial involves the use of anti-coagulants such as heparin.

As Zarychanski explains, patients with COVID-19 are at increased risk of blood clots, which appear to contribute to lung dysfunction. Blood clots are also inflammatory and heparin is known to be a potential anti-coagulant and anti-inflammatory agent.
As Research Today reported earlier this year, Zarychanski is leading two international clinical trials of therapeutic anti-coagulants with heparin. One study, known as the Anti-thrombotic Therapy to Ameliorate Complications of COVID-19 trial (ATTACC), is enrolling moderately ill patients admitted to hospital wards in Canada, the United States, Mexico and Brazil. The other study, known as the Randomized, Embedded, Multifactorial Adaptive Platform (REMAP), is enrolling critically ill patients in seven countries, including Canada, the United Kingdom, Ireland, Australia, New Zealand, Saudi Arabia and the United States.
These trials were recently merged and have been adopted by the United States as part of their national anti-coagulation trial. As a result, Zarychanski’s trial has developed into a large international collaborative trial designed to determine if anti-coagulation medication is effective in reducing mortality or the need for organ support. The study now involves as many as 150 senior clinical scientists like Zarychanski, as well as their respective teams. There are currently about 650 patients enrolled in the merged multi-platform trial around the world, and that number is expected to climb to about 1,000 to 2,000 by the time the trial reaches a conclusion.
“The idea is to get the answers (as to the effectiveness and safety of anti-coagulants like heparin) as soon as possible,” says Zarychanski, who has studied the effects of the medication for several years. In addition to receiving start-up funding from Research Manitoba, the project has also attracted funding from the Canadian Institutes of Health Research and the National Institutes of Health in the United States.
“The trial we started in Manitoba has grown beyond our wildest expectations,” he says of the collaborative effort.
Zarychanski says he cannot discuss the early results of the heparin trial that is now underway.
“We are going to have our first look at the data for effectiveness and safety by early November.”
But even then, Zarychanski expects it could several months before the team will conclusively know how effective heparin is in treating patients with COVID-19.
“Our plan is to stop the trial if there is overwhelming evidence that the treatment is helpful or not. The trial will continue until we know the therapy works or should be abandoned.”
While trials that could potentially identify an effective treatment for COVID-19 attract the most media attention, Zarychanski says scientists have also learned a lot from trials showing no benefit of a particular agent.
“Just because a drug doesn’t work doesn’t mean the trial hasn’t been successful,” he says.
A case in point is the trial that demonstrated that hydroxychoroquine was not useful for treating COVID-19 patients.
“It was important and responsible for us to find out that hydroxychloroquine was ineffective,” he says. The same can be said about the anti-viral Kaletra.
“Without this knowledge we would still be giving it to people based on political hype, emotional reaction, and good intention – while wasting time and money in the process. Of course, if a drug has no benefit, the likelihood of harm to patient also increases. Those are early successes for sure because they separated the wheat from the chaff.”
Repurposing existing drugs has been the focus of the early COVID-19 trials. In the next phase of trials, Zarychanski expects to see groups evaluating more targeted COVID-19 therapeutics, such as monoclonal antibodies or hyperimmune preparations. Identification of an effective vaccine remains and important goal. Several clinical trials are currently studying a number of candidate vaccines in the United States and elsewhere. Results may be announced as early as the end of 2020.
Brian Cole is a Winnipeg writer.